by Dorothée van Hooff | Mar 2, 2017 | Publications:
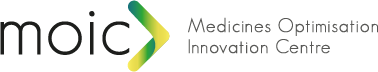
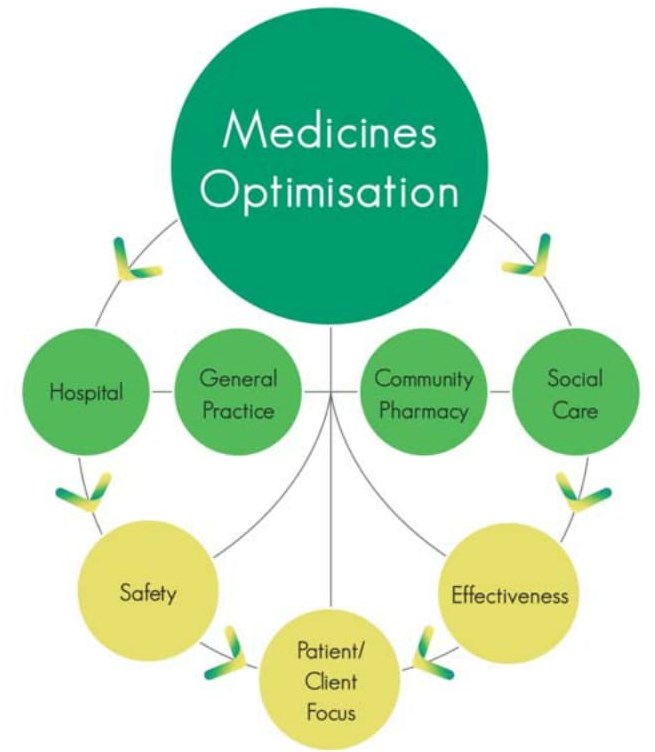
Medicines are the most common medical interventions within our population and, at any one time, 70% of the population is taking prescribed and over-the-counter medicines to treat or prevent ill-health. In simple financial terms, expenditure on medicines in Health and Social Care (HSC) in Northern Ireland is of the order of £ 550 million per annum. In addition, there is significant sub-optimal use of medicines resulting in sub-standard patient care and waste of healthcare resources. In order to address these issues a new approach is needed that moves the emphasis away from a system and service focus to a patient-focused medicines optimization (MO) methodology. To this end the Department of Health launched its policy document: the Medicines Optimisation Quality Framework (MOQF).
The MOQF has three strands: namely a regional MO model, quality standards, and a regional innovation plan. A key component of the policy was the establishment of a regional Medicines Optimisation Innovation Centre (MOIC). The MOIC will provide a focus for delivering a systematic approach to finding and resting solutions for the HSC in Northern Ireland.
In order to achieve its key aim of ‘smarter medicines, better outcomes’ the MOIC utilises the ‘quadruple helix’ approach as identified in the European Innovation Partnership in Active and Healthy Ageing, namely involvement of civil society, academia, healthcare and industry. This approach enables comprehensive inclusive solutions to be developed that meet the need of the population but with robust academic input as well as industry in the broadest sense in this regard.
Medicines Optimisation Innovation Centre (MOIC), authors: Michael Scott & Glenda Fleming. In: Journal of Medicines Optimisation (JoMO), Volume 3, Issue 1, March 2017
MOIC in Journal of Medicines Optimisation March 2017

by Dorothée van Hooff | Jul 6, 2016 | Publications:
The Spanish Society of Hospital Pharmacy (SEFH) has created a new initiative consisting of a scientific training exchange programme called “International Centres of Excellence in Hospital Pharmacy”. This programme consists of generating an internationale network which will connect leading-edge hospitals worldwide in the various areas of Hospital Pharmacy. The first international centre interested in cooperating and joining forces in the scope of the specialised training of post-graduates and in the furthering of research has been the Hospital Pharmacy Service of Antrim Area Hospital in Northern Ireland.
‘“International Centres of Excellence in Hospital Pharmacy”; a SEFH new initiative; the role of the clinical pharmacist in the hospital antibiotic stewardship in Northern Ireland’. Elena Alba Álvaro-Alonso, Mamoon Aldeyab, Linden Ashfield, Fiona Gilmore, Montserrat Pérez-Encinas. In: Farmacia Hospitalaria, 2016; 40(4): 233-236
Farmacia Hospitalaria SEFH Antrim Observership

by MOIC | May 22, 2015 | Publications:
The journey from medicines management to optimisation has resulted in significant improvements in the quality and safety of medicines yielding health gain and economy and a return on investment of £5–8 for each £1 invested. The complementary role of pharmacy in the multidisciplinary team has been identified and evidenced. The next steps will be to further integrate with primary care and deliver improvements in medicines processes in that sector together with requisite enabling technologies.
The optimisation of the medicines process has led to benefits to patients in terms of morbidity and mortality in addition to a reduction in healthcare resource utilisation. Key findings include reduced length of stay, reduced readmission rates, improved Medicines Appropriateness Index, improved Medicines
Administration Error rate, positive impact on Risk Adjusted Mortality Index and improved communication across the primary/secondary care interface. Enabling technology solutions were also implemented. The objective of this review is to assess the improvement in medicines processes in Northern Ireland focusing mainly on secondary care and at the interface with primary care and also to consider the benefits of enabling technologies for the system. The review was undertaken by examining all of the publications that had been produced together with relevant context articles that framed and supported the requisite process changes together with a synopsis of relevant enabling technologies that were devised. Key outputs were summarised and incorporated into the system review. ‘Integrated medicines management to medicines optimisation in Northern Ireland (2000-2014): a review’,
Michael G. Scott, Claire Scullin, Anita Hogg, Glenda F. Fleming, James C. McElnay. European Journal of Hospital Pharmacy (EJHP), May 2015, Volume 22, Issue 3
IMM to MO in Northern Ireland EJHP May 2015

by MOIC | Apr 19, 2015 | Publications:
‘An innovative approach to integrated medicines management’, Claire Scullin PhD, Michael G. Scott PhD, Anita Hogg BSc and James C. McElnay PhD. In: Journal of Evaluation in Clinical Practice ISSN 1356-1294. Accepted: 19 April 2006
Abstract: To determine whether an increased input by clinical pharmacists at each stage of the patient’s hospital journey, from admission through discharge, resulted in an enhanced level of patient care as measured by a number of clinical and economic outcomes.
Conclusion: The IMM service proved very effective and can be used as a template to support the implementation of comprehensive pharmaceutical care as a routine service across Northern Ireland and beyond.
JECP April 2006 An innovative approach to integrated medicines management

by MOIC | Sep 22, 2014 | Publications:
‘Enhanced clinical pharmacy service targeting tools: risk-predictive algorithms’, Feras W.D. El Hajji PhD, Claire Scullin PhD, Michael G. Scott PhD and James C. McElnay PhD. Journal of Evaluation in Clinical Practice ISSN 1365-2753. Accepted 17 September 2014.
Abstract: This study aimed to determine the value of using a mix of clinical pharmacy data and routine hospital admission spell data in the development of predictive algorithms. Exploration of risk factors in hospitalized patients, together with the targeting strategies devised, will enable the prioritization of clinical pharmacy services to optimize patient outcomes.
Conclusion: Algorithms created were valid in predicting risk of in-hospital and post-discharge mortality and risk of hospital readmission 3, 6 and 12 months post-discharge. The provision of ward-based clinical pharmacy services is a key component to reducing RAMI and enabling the full benefits of pharmacy input to patient care to berealized.
JECP Sep 2014 Enhanced clinical pharmacy service targeting tools riskpredictive algorithms