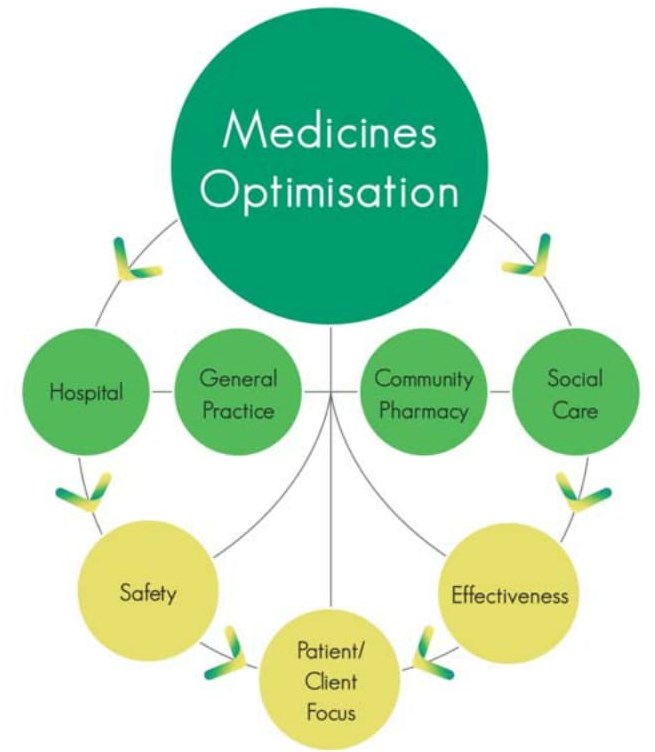
Medicines are the most common medical interventions within our population and, at any one time, 70% of the population is taking prescribed and over-the-counter medicines to treat or prevent ill-health. In simple financial terms, expenditure on medicines in Health and Social Care (HSC) in Northern Ireland is of the order of £ 550 million per annum. In addition, there is significant sub-optimal use of medicines resulting in sub-standard patient care and waste of healthcare resources. In order to address these issues a new approach is needed that moves the emphasis away from a system and service focus to a patient-focused medicines optimization (MO) methodology. To this end the Department of Health launched its policy document: the Medicines Optimisation Quality Framework (MOQF).
The MOQF has three strands: namely a regional MO model, quality standards, and a regional innovation plan. A key component of the policy was the establishment of a regional Medicines Optimisation Innovation Centre (MOIC). The MOIC will provide a focus for delivering a systematic approach to finding and resting solutions for the HSC in Northern Ireland.
In order to achieve its key aim of ‘smarter medicines, better outcomes’ the MOIC utilises the ‘quadruple helix’ approach as identified in the European Innovation Partnership in Active and Healthy Ageing, namely involvement of civil society, academia, healthcare and industry. This approach enables comprehensive inclusive solutions to be developed that meet the need of the population but with robust academic input as well as industry in the broadest sense in this regard.