by MOIC | Apr 28, 2016 | News Release
MOIC announces a partnership agreement with Pharmacy Management. The two organisations will work together to communicate and promote the development of medicines optimisation throughout the UK and beyond. More information: see profile Pharmacy Management.

by MOIC | Mar 3, 2016 | partners
The European Connected Health Alliance is the trusted connector in healthcare; we bring people, organisations, needs and solutions together. We are a Community Interest Company (not-for-profit) registered in Northern Ireland. ECHAlliance exists to facilitate multi-stakeholder connections, to create and strengthen partnerships committed to driving sustainable change, in the quality and efficiency of health and social care.
With over 15,000 connections across Europe, North America and China, we are a powerful international force for change, whose combined knowledge, expertise and connections can speed up progress. We work through our International Network of Permanent Ecosystems, an unparalleled network connecting more than 25 multi-sector Ecosystems, each of which brings together a community of stakeholders interested in developing a joint health agenda, relevant to their respective country or region.
Our primary functions are:
- Promotion of connected health – to provide leadership, education and focus supporting European and global implementation of connected health technologies.
- Development of connected health capabilities – to secure and engage in collaborative R&D.
- Participant and member support – to support the strategic and tactical marketing and business development needs of ECHAlliance members.
- Education – to develop and provide educational opportunities, in support of broad scale deployments connected health.
As part of our drive to achieve these primary functions ECHAlliance developed a range of inter-Ecosystem working groups focusing on priority areas highlighted through the network. Medicines Optimisation was identified as a priority area for many Ecosystems and we launched the Medicines Optimisation Working Group (MOWG) in October 2015. We are delighted that Professor Michael Scott, Director of the Northern Ireland Health Medicines Optimisation Innovation Centre (MOIC) will Chair this international group. MOWG acts as a forum to test thinking, share best practice and provide advice on developments; we will work with MOIC as part of the network to support combined knowledge and expertise to propel progress.
More information: https://echalliance.com/

by MOIC | Mar 2, 2016 | News Release, Press
Today Health Minister Simon Hamilton launched the NI Medicines Optimisation Quality Framework at the MOIC. Minister Hamilton announced at the same moment a £30m Transformation Fund, and confirmed £300k recurrent funding for MOIC from this Fund.
(From left, Simon Hamilton, Health Minister; Dr Tony Stevens, Chief Executive NHSCT; Prof Mike Scott, Director MOIC)
For more information: https://www.dhsspsni.gov.uk/consultations/medicines-optimisation-quality-framework
by MOIC | Mar 1, 2016 | Products
Electronic Pharmacist Intervention Clinical System
Patient safety in Northern Ireland can be enhanced via the use of EPICS (Electronic Pharmacist Intervention Clinical System). This novel software package, designed in conjunction with a local software company, enables pharmacy staff to record in real-time their clinical activities and clinical interventions (any action taken to correct a problem identified in a patient’s medications). These recorded interventions are archived for subsequent analysis. NHS data standards such as the dictionary of medicines and devices (dm+d) and the National Patient Safety Agency (NPSA) risk matrix are already fully integrated into EPICS and the software is designed to be compatible with NHS computer systems UK-wide.
Learning from data
EPICS provides an agreed, comprehensive, consistent approach to recording clinical pharmacy data in a digital format. This standardisation of data ensures that every user is recording the same information in the same way at every site, while the paperless format helps to protect confidentiality and avoid data loss. This combination of both uniformity of approach and digital format means that data can be analysed quickly and easily at both local and regional level to allow meaningful benchmarking. With this in mind a suite of reports is available which can analyse the data at both the quantitative and qualitative levels.
EPICS can be linked to hospital incident reporting systems (e.g. DATIX) to improve learning from critical incidents in line with NPSA best practice. EPICS is designed to identify problem medications, the early detection of emergent trends, and to promote systemic learning so that ‘… the risk of avoidable harm to patients is minimised’ in line with the aspirations of An organisation with a memory.
Four of the five Healthcare Trusts in NI are already using EPICS. Work is currently on-going to extend the reach of EPICS into community pharmacies in primary care. This will make clinical governance and medicines management tools available to pharmacists across the healthcare continuum in both primary and secondary care. This extension would ensure a fully integrated optimal medicines management system utilising standard technologies. This would have significant benefits for improving safety & quality of patient care, continuity of service and health analytics.
by MOIC | Mar 1, 2016 | Products
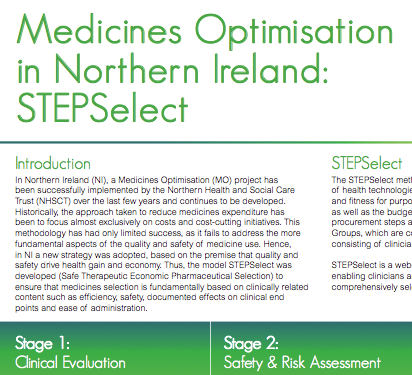
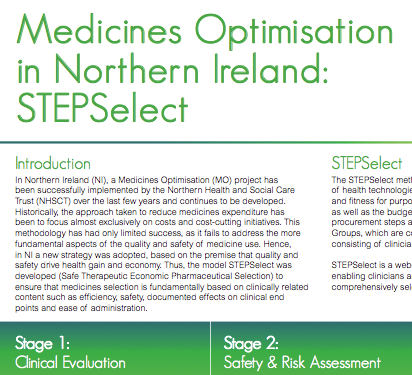
Historically, the approach taken to reduce medicines expenditure has been to focus almost exclusively on costs and cost-cutting initiatives. This has had only limited success, as it fails to address the more fundamental aspects of the quality and safety of medicine use.
In conjunction with our collaborators, the STEPSelect programme (Safe Therapeutic Economic Pharmaceutical Selection) has been developed. This system ensures that medicines selection is fundamentally based on clinically related content such as efficacy, safety, documented effects on clinical end points and ease of administration. STEPSelect is a web based tool developed by Digitalis Mm Ltd, enabling clinicians and other health care providers and managers to comprehensively select and procure medicines and medical devices.
Transparent process
The STEPSelect method looks in first instance at clinical features of health technologies. At a later stage of the evaluation, product quality and fitness for purpose are assessed (the so-called risk assessment stage) as well as the budget impact of a health technology and appropriate procurement steps and routines. Evaluations are carried out by Expert Groups, which are composed on the basis of a multidisciplinary nature consisting of clinicians, pharmacists, nurses and other staff as appropriate. The STEPSelect method has been used for a number of drug classes including erythropoietin stimulating agents and granulocyte colony stimulating factors and has now been extended to include dressings and medical and surgical devices. The outcomes of the process are used to produce guidance and to assist in formulary management. This can then be used to inform electronic decision support at the point of prescribing.
Stage 1: Clinical Evaluation
- Literature evidence compiled by professional editorial network of Digitalis
- Review evidence supplied by Pharmaceutical Industry, additional to the literature review (STEPSelect) and best evidence
- Assign relative weights to each selection criteria and scores to each product
- Ranking of chemical entities to proceed to Stage 2
Stage 2: Safety and Risk Assessment
- Product samples obtained from Industry
- Assessed using modified versions of national QC and Risk Assessment tools for Medicinal Products: Product Quality and Fitness for Purpose (PQFFP) and Medicines Error Potential Assessment (MEPA)
- PQFFP (Pass/Fail); MEPA (Low, Medium, High)
- Ranking of chemical entities and MEPA scores to proceed to Stage 3
Stage 3: Budget Impact Analysis
- Annual usage data obtained to allow comparison of products within the same class
- Ranking of chemical entities to proceed to Stage 4
Stage 4: Contract & Guidance
- Guidance produced to inform the service of products suitable for prescribing first line
- Relevant contracts put in place
Efficiency gains
In NI the STEPSelect technology has been applied to procurement of medicines in many different therapeutic groups such as statins, erythropoietin stimulating agents (ESA’s) and the use of biologicals in rheumatoid arthritis. Results with the method have invariably been positive in terms of support by clinicians and quality and cost reductions of prescribing, often in the region of 20-25% per therapeutic group.
Benefits:
- Reduced medicines related adverse events
- Improved Quality: Drug selection based on safety & efficacy, then cost
- Improved Efficiency: Cost-effective drug selection, reduced stockholding and reduction of out of date stock
- Robust, transparent, defensible process
Interactive website:
- Tablet devices for Expert Group members
- Project mentor
- Project key for limited access for special target groups
- e-Sessions to highlight choices for special interest groups
- Comprehensive stakeholder input via these interactive mechanisms
Summary:
- Supports a clinical driven procurement process
- Process is based on the principles of quality and safety
- Supports guidance and formulary development and maintenance
- Maximises health care resource utilisation
- A key component of Medicines Optimisation
MOIC STEPSelect Poster